A proposed federal policy intended to improve access to opioid addiction treatment may not have much of an impact in St. Louis.
The rule change would allow doctors to prescribe a medication that reduces withdrawal and cravings to twice as many patients.
But two of the largest treatment providers in St. Louis say their doctors aren’t in danger of exceeding the current 100 patient-limit for buprenorphine, a drug often trademarked as Suboxone.
“I think it’s a good change for our organization, and it’s just a good change, period,” said Mike Morrison, vice-president of Preferred Family Healthcare. “In our case it’s not as much of an issue because although we have quite a number of people that are on a longer-term, more of a maintenance dose — and by that I mean like a year or so — a lot of our medical director’s patients are there for detox.”
Morrison is the former director of Bridgeway Behavioral Health, the only state-funded, medication-assisted in-patient detox center in Eastern Missouri. Bridgeway merged with Preferred Family Healthcare in January. The combined organization sees about 8,000 patients a year.
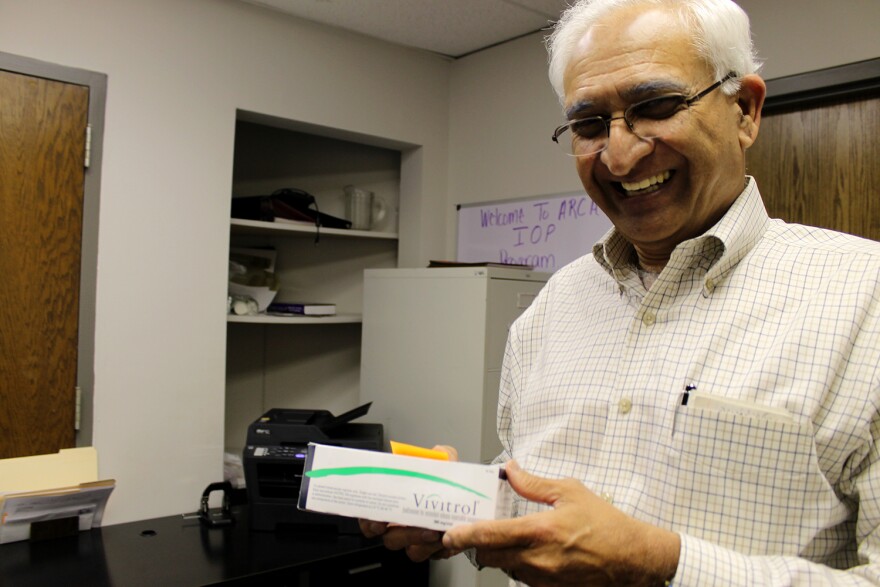
Assisted Recovery Centers of America, another large St. Louis addiction treatment provider, uses Suboxone exclusively for detox.
ARCA President Percy Menzies said the proposed buprenorphine policy change won’t have much of an impact on his clinic.
“We keep them on it for a short time, detox them. Then we offer them other treatment. That’s why our physician slots are pretty open,” said Menzies, a proponent of a non-addictive medication called Naltrexone, which blocks the opioid receptors in the brain and prevents a user from feeling the effects of a high.
Both Morrison and Menzies said other policy changes would have a greater impact than the proposed buprenorphine rule.
Morrison said Preferred Family’s doctors may eventually need to take advantage of an increased buprenorphine prescription limit, but a policy increasing the number of beds allowed in clinics that take Medicaid would have a much greater and more immediate effect.
“If they would do away with the IMD rule, that would probably be the biggest thing that could happen for us,” Morrison said.
The Medicaid Institutions for Mental Diseases Rule, or IMD, limits facilities to 16 beds even if they have the space and staffing to support more. It was intended to make sure that people with mental illnesses weren’t warehoused in large psychiatric hospitals.
“It certainly alleviated one issue but it’s caused us a tremendous headache and really left a lot of people out in the cold,” said Morrison.
Menzies said he would like to see buprenorphine, which is an opioid, treated like opioid painkillers.
“Any physician with a license can prescribe the most super heavy-duty pain medications including fentanyl, oxycodone without any restrictions. But we are facing these restrictions on buprenorphine. It doesn’t make any sense,” said Menzies.
Right now doctors have to sign up and pass a test in order to prescribe buprenorphine. Menzies believes removing that requirement would help remove silos and help mainstream addiction treatment.
“I go to the primary care physician for my other illness, for my hypertension, diabetes and things of that sort. When it comes to my opiate addiction I go to a different physician. So this will break down the silos,” said Menzies.
In order to prevent over-prescription, Menzies would change buprenorphine to a schedule 2 drug, which requires face-to-face contact with a patient. He believes that personal relationships with patients will help them receive better care and get connected to behavioral therapy that helps them address the root of their addiction.
Follow Camille Phillips on Twitter: @cmpcamille.





